Clinical perfusionists: working behind the scenes
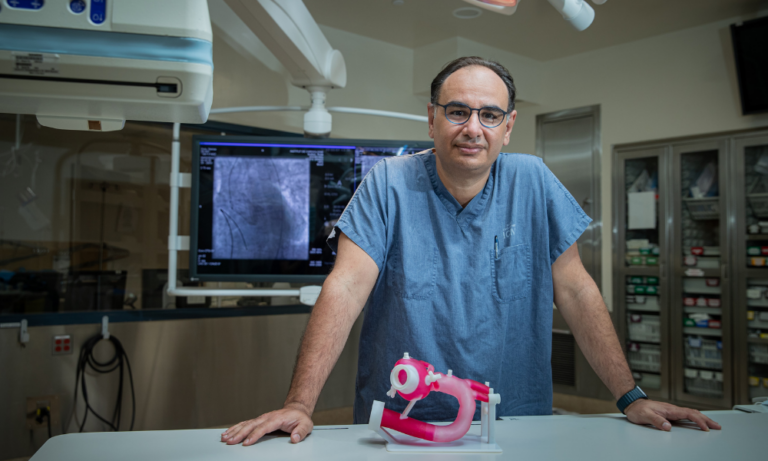
Interview with Hosham Ased, clinical perfusionist at the Montreal Heart Institute
Home > Blog > Clinical perfusionists: working behind the scenes
This article is adapted from the third edition of the Foundation’s magazine
“With the help of external equipment, we keep the blood flowing and keep the body alive during surgery that requires the heart to be free of blood. We reproduce the human physiology and replace the functions of the heart and lungs to ensure they’re well oxygenated.”
The recipient of the third edition of the Dr. Denis Roy Awards for Excellence in Cardiovascular Care, Hosham Ased is an ambassador of his profession. He works tirelessly to help advance the practices used in his field, and below he talks about the little-known yet critical role of clinical perfusionists.
From engineer to clinical perfusionist—a natural progression
It was back in 2006, when he was working towards a bachelor’s in biomedical science with the aim of specializing in engineering, that Hosham Ased first learned about the profession of perfusionist. “A colleague of mine at the time was doing an internship in perfusion, and he said, ‘Come see, we’re in the operating room—it’s lively, we have contact with the patients, there’s lots of adrenaline, and we play a valuable role.’ It piqued my curiosity, because in biomedical engineering, there’s no direct contact with patients. I was immediately intrigued by the balance between developing technologies and working closely with medical practitioners,” he explained
While working towards a master’s degree in biomedical engineering, Hosham discovered just how appropriate his career path was, despite an apparent disconnect: “I learned that the first perfusionists to work at the Montreal Heart Institute, where I was doing my engineering internship, were also engineers by training. Understanding how the human body works coupled with technological know-how is a major asset. Given that the aim of a biomedical engineer is to leverage innovation to improve patient care, the decision to work more closely with patients by becoming a clinical perfusionist once I had finished my master’s degree was a natural transition for me,” he said.
Maintaining the body’s vital functions during surgery
Since 2011, Hosham has been part of the team of perfusionists at the Montreal Heart Institute. Every day, he monitors machines that keep the patient’s blood flowing and organs functioning during complex surgeries.
“We divert the blood from the heart so it can be repaired. Same thing for the lungs, to clear the passageway and make it easier to operate. The aim is to remove the blood from the area being operated on. This gives the surgeon more time to operate. Before perfusion was introduced, you had to hurry to avoid damage to the vital organs. It was risky and the margin of error was huge,” he explained.
A clinical role focused on creativity and collaboration
Working in the background, perfusionists spend most of their time in the operating suite: “We enter the picture once the patient is under anesthesia. We work in tandem with the surgeon. There’s a true synchronicity between the two specialties—it’s like two musical instruments playing off each other. The perfusionists at the Montreal Heart Institute have known each other for a long time. When complications arise, we rely on each other. We don’t even have to say a word—we just know. The ties that bind us are very strong.”
Advancing clinical perfusion practices through knowledge transfer
In recognition of his outstanding contribution to the advancement of his profession, Hosham was honoured with the Dr. Denis Roy Award for Excellence in Cardiovascular Care, highlighting the extent of his efforts. “I’m heavily involved at the Institute because I’ve always wanted to have an impact, make a difference, and make strides in the field. My longing to share my knowledge and drive innovation is what continues to inspire me,” he said.
Since 2013, Hosham teaches in the clinical perfusion program at Université de Montréal, where his engineering expertise is recognized and valued. As clinical coordinator and monitor at the Montreal Heart Institute, he oversees the practical training of young perfusionists. “It allows me to explore a side of myself that loves to communicate, to share. I also believe that the best way to understand and master a practice and stay up to date on what’s happening in the field is to teach,” he noted.
“In my teaching, I value contact with different specialties, because they can all help advance the perfusion practice. In this profession, there’s a lot of room for creativity and problem-solving, dealing with the unexpected and making quick decisions, since every situation is unique and our care approach needs be adapted to each individual patient,” he added.
Innovative research projects to benefit patients
Constantly pushing the boundaries of his discipline, Hosham is currently completing a doctorate on the strategies to minimize hemodilution during extracorporeal circulation.
“I’m looking to reduce the circuit, meaning the length of the tubes the blood flows through outside the body. The goal is to achieve extracorporeal circulation in which red blood cells don’t get diluted—where no physiological liquid has to be given to the patient. This would prevent the need for post-operative blood transfusions, which can have negative health effects. Ultimately, we’d only use the patient’s blood for extracorporeal circulation, in a very short circuit,” he said.
In June 2022, Hosham was invited to a symposium of perfusionists in Saint-Malo, France—a sign that his work has reverberations around the world. “The French want to use the model we built here and the deep expertise we’ve developed in clinical perfusion over the last 15 years. We’re on the leading edge because we have access to advanced technology and we’re continuously honing our skills. I’m proud to help boost the Institute’s international reputation in a field I love and, more importantly, to leave my mark here by making a real difference, one patient at a time.”
Want to help improve care? Help the Institute’s experts push the limits of what is possible.
Donate today