Echocardiography: A window into what the eye can’t see
Interview with Dr. André Denault, anesthesiologist and critical care physician at the Montreal Heart Institute
Home > Blog > Echocardiography: A window into what the eye can’t see
This article is adapted from the third edition of the Foundation’s magazine
“Every week, there’s at least one patient whose surgical plan will completely change because of their echography or ultrasound. These images allow us to take appropriate action and see what a typical physical exam can’t show us.”
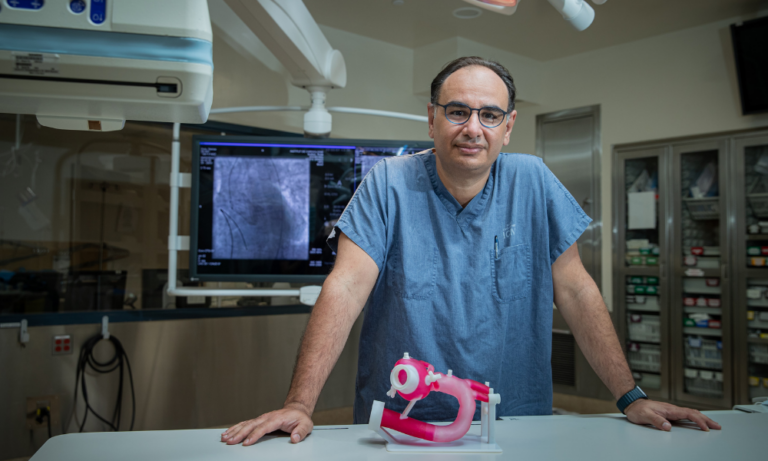
Since the beginning of his career, Dr. André Denault, anesthesiologist and critical care physician at the Institute, has been interested in ultrasounds’ exceptional potential for treating patients. This world specialist in cardiac anesthesia was excited to speak to us about the practice he implemented at the Institute that revolutionized the way medical professionals around the globe make diagnoses.
Discovering the extraordinary potential of ultrasounds
Dr. Denault first learned about echocardiography during his internal medicine residency in 1989. “Someone was going into cardiac arrest—the situation was critical. The chief cardiologist made an urgent request for an emergency ultrasound. The images gave us information about the patient’s condition in a non-invasive way and allowed us to make an informed diagnosis. I was fascinated. That’s when I knew that I had to learn how to use this incredible tool.”
Wanting to specialize in intensive care, Dr. Denault completed a two-year fellowship in Pittsburgh. That’s where he first came across transesophageal echocardiograms (TEE). “When the images taken from the surface of the body are inadequate, or if this is simply not possible, instead of putting the ultrasound on the thorax, it can be inserted into the esophagus and placed right behind the heart. This produces amazingly clear images. In 1991, we were only just starting to perform this type of echocardiography. I remember thinking, ‘This is the future. It’s going to be used all the time in operation rooms and intensive care.’ It’s a precious opportunity to understand what’s going on with a patient.”
An innovative practice at the Montreal Heart Institute
Dr. Denault was invited to join the Montreal Heart Institute in 1999. That same year, in collaboration with Dr. Pierre Couture, he fulfilled the task of bringing the practice of TEE to their operating rooms. He’s proud of how far they’ve come in the last 25 years.
“Today, every single anesthesiologist at the Institute is trained in doing ultrasounds. About 40,000 TEEs have been done to date. We now have cutting-edge ultrasound equipment in our seven operating rooms—there’s no place better equipped for helping patients.”
According to Dr. Denault, the implementation of echocardiography to the Institute inspired new methods that are now used globally. “The fact that the anesthesiologist is getting images in real time enables a closer relationship between them and the surgeon—they’re in constant communication before, during and after the operation, which leads to better decision-making. Doctors from around the world come here to train in cardiac anesthesia so they can learn from the expertise we’ve developed over the years thanks to this tool. We’ve become a model in this field.”
Targeted ultrasounds: The fifth pillar of physical exams
Using ultrasounds to examine patients unlocks a potential that goes beyond the heart alone. Dr. Denault believes that targeted ultrasounds—which allow physicians to evaluate a person’s lungs, abdomen, brain, blood vessels, and more—will become a universal practice in critical care.
“It’s a mini revolution in the art of physical examination. Insonation is becoming the fifth pillar, adding to inspection, palpation, percussion and auscultation when performing a general patient evaluation. Modern ultrasound devices produce images that allow us to determine with certainty what’s going on in all parts of the body.”
Training healthcare professionals to do ultrasounds
These promising avenues led to the development of new training opportunities at the Institute, as well as the founding of the Centre de formation et d’excellence en santé cardiovasculaire (Cardiovascular centre for training and excellence) in 2022. “Among other things, the Foundation has given us these amazing ultrasound simulation tools to help train professionals and students. Many doctors come to the Institute to take advantage of our ultrasound simulation centre. They can observe more simulated pathologies in a single day than they’ve ever seen in their entire career. It’s vital when you’re trying to make an accurate diagnosis.”
Research on ultrasounds, with support from the Foundation
Thanks to the Foundation’s donors, anesthesiologists and researchers alike benefit from the support needed to learn more about ultrasounds. “We have a lot of research to do to uncover the full potential of this practice. Every year, I can rely on the Foundation’s invaluable help to pursue projects that improve patient care.”
Dr. Denault is enthusiastic about all the ways ultrasounds will be used in the future. “Physiotherapists already use it in their own practice to observe the lungs and musculoskeletal injuries. Family doctors could use it in outpatient clinics to help them make better diagnoses. Nurses could use it to find a vein before inserting a needle. There are so many situations where we’ll be able to observe before intervening, and the patient will be better for it.”
Help improve care for those affected by cardiovascular disease.
Donate